Physio for Knee Pain, Common Conditions and Treatments
Overview
The knee joint is one of the most complex and unique joints in the body. It is one of the most overworked joints simply on the fact that approximately 70% of ones body weight lies above the knee. The complex structure is made up of bones, cartilage, tendons, and ligaments that are prone to tears, fractures, sprains, and degeneration. Every action, step, or movement utilizes the knee joint and surrounding musculature in some capacity. This means, unfortunately, irrelevant of your level of activity, structure or size, knee pain can affect almost anyone. In this article we will discuss why you should consider physio for knee pain.
Understanding the joint, its structure, biomechanics, and ultimately how to put stresses through it safely, is crucial.
The knees rely on quadriceps, which contain four muscles: rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis. The muscles as the back of the thigh called the hamstrings also refer to another group of muscles: semi-tendinosus, semi-membranosus, and biceps femoris. Hip abductors, glute muscles, and calf muscles also work together to stabilize the knee joint. Strengthening these muscles can help alleviate the daily weight-bearing stresses experienced by the knees.
Going on walks, using the stairs instead of the elevator, or riding a bicycle are all great forms to promote knee health. This is because extended periods of inactivity cause soft tissue to become tight and weak which could lead to various other conditions associated with disuse.
Knee Anatomy

There are four main bones which make up the knee joint:
Femur: The femur is the longest bone in the body and is a ball and socket bone. It runs from your hip to your knee.
Tibia: This bone is one of the two that make up the lower leg. It is the longer of the two bones within your shin. It is located on the inside of your leg and is the primary bone of weight bearing with all movements.
Fibula: This is the other and shorter bone of the lower leg. It is located on the outside of your knee and makes up for only about 15% of weight bearing.
Patella: The patella is also more commonly known as your knee cap. It is an oval shaped bone that lies on your femur and helps provide protection to the front of your knee.
In addition to bony anatomy, the knee consists of 4 main ligaments: Medical Collateral Ligament (MCL), Lateral Collateral Ligament (LCL), Anterior Cruciate Ligament (ACL) and Posterior Cruciate ligament (PCL) which help stabilize the knee join in all 4 cardinal planes.
In between all bones lies cartilage to prevent the grinding of bone on bone and to provide for soft and smooth movement. In between the cartilage we have menisci known as the shock absorbers of the knee The meniscus are cartilaginous structures which are C shaped and help provide extra cushioning of the knee joint. They are located between the Femur and Tibia on both ends to help provide shock absorption. Each knee joint has two menisci, one that is located on the outside of the knee joint (lateral meniscus) and one the is located on the inside of the knee (medial meniscus).
Types of Knee Injuries
Based on its function and overall weight bearing the knee joint is prone to many types of injuries. These include:
Acute injuries : Occurs 1-7 days post injury. Most severe pain. Acute injuries occur typically from some specific injury, whether it be a sport injury, a slip and fall, planting ones foot incorrectly, etc.
Sub-acute injuries: 2-6 weeks after acute injury. The injury has been unaddressed and pain and limited mobility continues to linger with certain movements and actions of the knee.
Chronic injuries: Greater than 8-12 weeks. If further left unaddressed, an acute —> sub-acute injury can develop into a chronic pain problem. Meaning the body is recognizing that this issue is not resolving in turn sending more pain signals to the brain to warrant action. Chronic pain however can also arise from degenerative changes left unaddressed for years.
Types of Diagnoses
Patellofemoral Pain Syndrome (PFPS):
Patellofemoral Pain Syndrome (PFPS) is an umbrella term used for pain arising from the patellofemoral (patella + femur) joint itself, or adjacent soft tissues. It is a chronic condition that tends to worsen with activities such as squatting, sitting, climbing stairs, and running. It is also referred to as “runners knee” or “jumpers knee” due to the high incidence in runners and athletes developing this condition. In most cases of PFPS, the pain is a dull achy pain that is located in the front of the knee or around the knee cap, worsened during a squat/lunge. The patient will often describe it as pain “under or around the knee cap”.
Typically, the main cause of PFPS comes from intense athletic involvement, or it may stem from an alignment issue of the knee resulting in excessive forces being transmitted through the knee joint and around the knee cap.

Meniscal Injuries

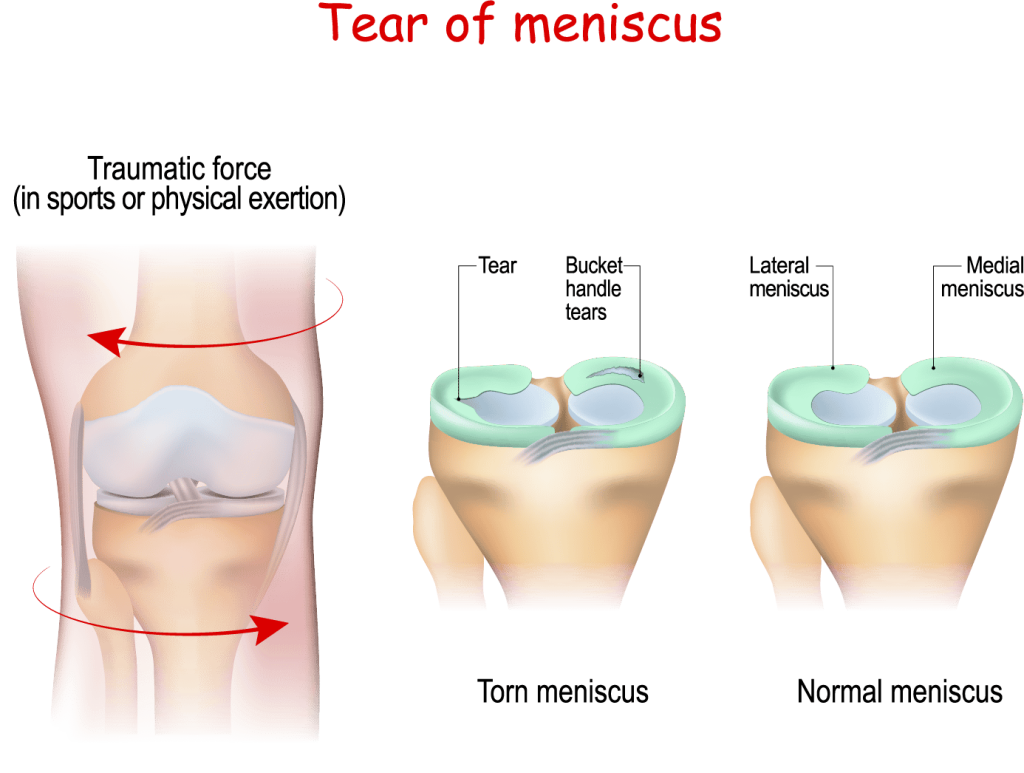
As described above , the meniscus acts as the shock-absorber of the knee. Therefore, if the amount of shock or load going through the knee exceeds the amount of shock the meniscus can sustain, this may result in a meniscal tear. The symptoms of a meniscus tear are a sharp pain either on the inside or outside of your knee (where the menisci sit), an inability to bend your knee due to clicking or locking, and notable swelling.
This type of injury most likely occurs if you are twisting your knee quickly while your foot is on the ground and your knee is bent. This type of motion usually occurs with those who are involved in sports or those who are lifting heavy weights and have their knees in the position mentioned above. For example, a basketball player landing from a rebound, or a soccer player turning with a planted foot in the turf
Knee Osteoarthritis (degeneration)
Osteoarthritis (OA) of any joint is simply degeneration over time of the cartilage that sits at the end of each of the long bones. Degeneration of the knee can occur for various reasons such as: being over weight, previous injuries creating poor biomechanics in the knee, frequent overuse and overload positions or actions of the knee.
Osteoarthritis, commonly known as wear-and-tear arthritis, is a condition in which the natural cushioning between the joints’ cartilage wears down. When this happens, the bones of the joints rub more closely against one another with less of the shock-absorbing benefits of cartilage. The rubbing results in pain, swelling, stiffness, decreased ability to move and, sometimes, the formation of bone spurs.
Once the cartilage begins to wear down a patients pain will typically increase. The symptoms of knee osteoarthritis are swelling, sharp or achy pain, locking of the knee joint, and pain that is usually worst after a bout of rest.
Osteoarthritis is the most common type of arthritis. While it can occur even in young people, the chance of developing osteoarthritis rises after age 45. According to the Arthritis Foundation, more than 27 million people in the U.S. have osteoarthritis, with the knee being one of the most commonly affected areas. Women are more likely to have osteoarthritis than men.
Most common factors causing OA of the knee:
- Age (>45 means increased risk)
- Weight (follow BMI chart)
- Heredity (genetic influence)
- Repetitive stress injuries (years of the same stresses in the joint)

Collateral ligament injuries (ACL/PCL/LCL/MCL)
Each of the above ligaments (attaching bone to bone) provide stability to the knee:
The anterior cruciate ligament prevents the femur from sliding backward on the tibia (or the tibia sliding forward on the femur).
The posterior cruciate ligament keeps the shinbone from moving backward too far. It is stronger than the anterior cruciate ligament and is injured far less often.
The lateral collateral ligament is a ligament on the outside of your knee. It connects your thighbone to the bone of your lower leg and helps keep the knee from bending outward.
The medial collateral ligament connects the bottom of the thighbone (femur) to the top of the shinbone (tibia). The MCL helps keep the knee from moving side to side.
Typically ligamentous injuries in the knee require some type of significant force to the knee either directly, or indirectly through forces exerted above (hip or higher) or below (ankle/foot). Depending on the severity of injury, ligamentous injuries can be fixed with physiotherapy treatment or may require surgery. To that point, a smaller grade injury if left untreated can become a higher grade injury making recovery more difficult and/or requiring surgery.

Treatment for knee injuries or pain
Every treatment for knee pain or dysfunction will be different and customized to your symptoms and condition. Various factors are taken into consideration when designing a treatment protocol to each patient which include: the mechanism of injury, level of activity/inactivity, age, severity of injury.
At Physio Pros, our physiotherapists take the time to understand your specific situation to determine the best diagnoses and treatment options. Our focus is a hands-on manual therapy treatment approach in every session to get you moving and feeling better as fast as possible.
Your initial examination results and your commitment to treatment determine the duration and frequency of your treatment plan. The plan is designed specifically to your needs and will be progressive and change based on the results as you progress through treatment. The initial examination will consist of:
- Subjective and objective discussion of current injury and state
- Physical testing of strength, range of motion, and tolerance to movement
- Balance testing, gait analysis
- Special tests deemed necessary
Once an appropriate diagnosis is made and a plan is put together we will commence our first treatment on the same day. Typically, in house treatment will include a hands-on manual therapy treatment approach with the use of various modalities : electrotherapy, laser therapy, ultrasound, massage gun, heat/cold therapy.
Bracing – In many instances it is appropriate to brace the knee to increase stability around the joint, increased compression (to decrease swelling), and shift weight away from the damaged area of the joint.


In most instances, patients will be given homework assignments around strengthening and stretching which may include:
- Quad stretches
- Calf raises
- Squats / lunges
- Hamstring strengthening/stretching
- Glute strengthening
- Balance exercises
How long will it take to get better if I use physio for my knee pain?
As mentioned earlier, each type of knee injury has a unique mechanism of injury and is always unique to each client. Thus each individuals recovery will be different. However typically the state of injury (ie: Acute/Sub-acute/Chronic) as well as the severity of injury (ie: grade 1 vs grade 3 ligament tear) can often give us a rough idea how long it will take for an individual to feel better.

A typical timeline may follow these guidelines:
Acute: Most severe pain. Occurs 1-7 days after injury. Use R.I.C.E. (rest, ice, compression, elevation) before beginning regular activity. Recovery may take 3-6 weeks (or longer).
Sub-acute: 2-6 weeks after injury. Mild but noticeable pain that is not going away. Start physiotherapy to regain motion, manage pain and optimize strength with the knee. Recovery time may take 4-8 weeks (or longer).
Chronic: Greater than 8-12 weeks. It is time to speak with a health care professional and begin a treatment plan as soon as possible. Chronic pain can become more complex to treat and will require active engagement from the patient day-to-day. Recovery time may take 8-12 weeks (or longer).
Note, typically the more chronic (more time has passed) a condition is the more time it will take to show improvements in movement, reduced pain and increased range of motion. Therefore it is very important to remember not to let conditions worsen but to have them addressed as quickly as possible.
Key factors leading to best treatment outcomes:
- Consistency attending physical rehabilitation, particularly in the early phases.
- Active engagement/commitment from patient (for ex: home exercises).
- Avoiding similar activities that have lead to current state/injury
Physiotherapy at Physio Pros
At Physio Pros, we pride ourselves on our unique patient-centred approach to physiotherapy. We provide only one-on-one physiotherapy sessions because we believe every patient deserves our full attention and expertise.
Your confidentiality and privacy are of the utmost importance, and therefore your hands on treatment sessions always take place in confidential and private therapy rooms.
We look forward to the opportunity to serve you and to get you back to doing the things you love!